2019 BLACK FRIDAY SPECIAL OFFERS
Forget the Black Friday Madness and Pamper Yourself with Botox!
— VALID ONLY ON FRIDAY, NOVEMBER 29, 2019 —
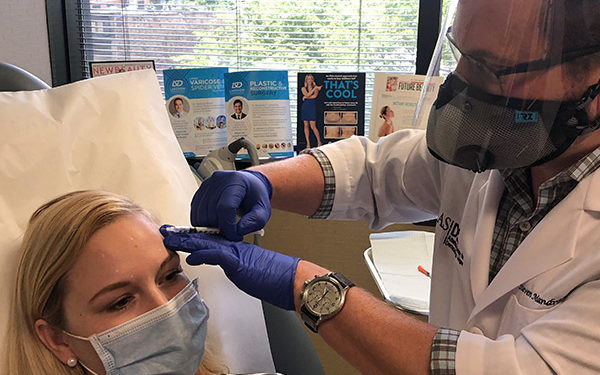
BOTOX® Cosmetic is a short and minimally invasive treatment that requires no downtime. During treatment, very low doses of botox are administered by way of small injections directly into the muscles that cause the frown lines between the brows and above the brows as well as the crow’s feet around the eyes. It can also reduce some lines on the lower lids, the bunny lines on the nose and the downward pull of the angles of the mouth.
BOTOX $12/unit (reg. $15/unit) with
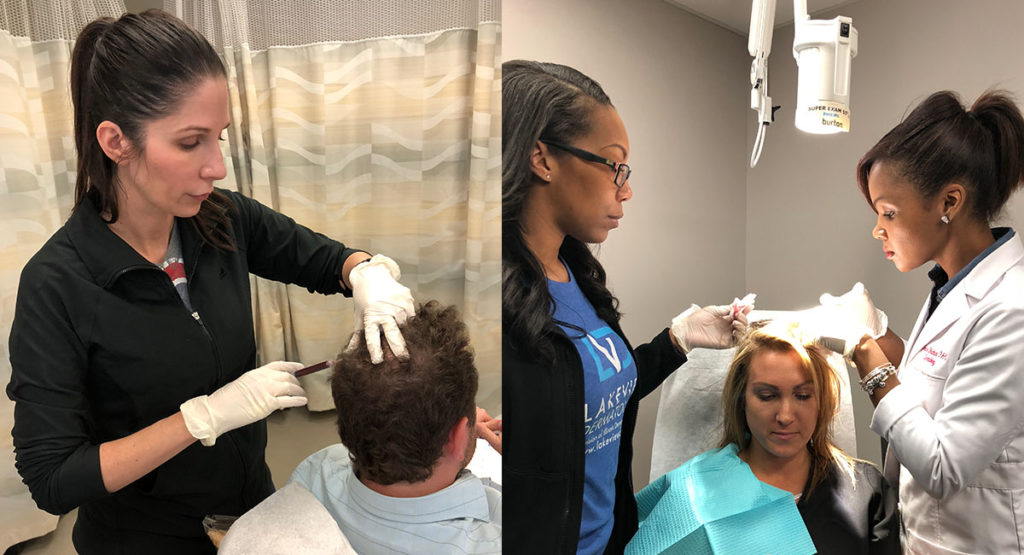
Jang Mi Johnson, PA-C in Chicago Lakeview Location

Jang Mi Johnson, PA-C graduated from the Cook County Hospital/ Malcolm X College Physician Assistant Program in 2002, the oldest and one of the most competitive programs in Illinois. She is nationally certified by the National Commission on Certification of Physician Assistants (NCCPA) and licensed by the state of Illinois. Her interests include Multicultural hair and skin, pediatric dermatology, psoriasis, acne, cosmetic skin treatments, and many other common skin conditions.
Please call 773-281-9200 to book your BOTOX treatment with Jang Mi Johnson, PA-C.
BOTOX $12/unit (reg. $15/unit) with
Tracee Blackburn, PA-C in Palos Heights Location

Tracee Blackburn, PA-C is a Board-Certified Physician Assistant, nationally certified by the National Commission on Certification of Physician Assistants (NCCPA) and licensed by the state of Illinois. She has specialized as a PA in Dermatology since 2005. Tracee graduated from Midwestern University in Downers Grove, Illinois in 2005. She has worked in several entities of healthcare, but found her passion in Dermatology where she has extensive experience in general, surgical, and aesthetic dermatology. She diagnoses and treats common dermatologic conditions, is proficient in detecting and treating skin cancers, performs basic and intermediate surgical procedures, and performs cosmetic and laser services. Her special interests are acne, eczema, psoriasis, benign skin lesions, and skin cancer. Tracee likes to focus her attention on patient education, as she believes it is a vital part to every patient’s recovery.
Please call 708-671-1374 to book your BOTOX treatment with Tracee Blackburn, PA-C.
BOTOX $12/unit (reg. $15/unit) with
Susan Heemstra, RN in Palos Heights

Susan Heemstra, RN has been in dermatology for over 35 years, working side by side with Dr. Eugene Mandrea, and performing lasers for more than 13 years. She has attended numerous laser training events, including Harvard University’s laser convention. Sue provides laser treatments for many conditions including acne and acne scars, rosacea, wrinkles, age spots, skin laxity, tattoo removal, spider veins, and hair removal. She enjoys working with our medical staff to develop laser plans that address medical as well as cosmetic concerns. In addition to laser treatments, Sue is also experienced at Botox injections, Coolsculpting, tumescent liposuction anesthesia and assisting with skin cancer surgery.
Please call 708-671-1374 to book your BOTOX treatment with Sue Heemstra, RN.
BOTOX $12/unit (reg. $15/unit) with
Brittany Scurto in LVD Park Ridge Location

Brittany Scurto, PA-C is a board-certified Physician Assistant, nationally certified by the National Commission on Certification of Physician Assistants (NCCPA) and licensed by the state of Illinois. She graduated from University of Illinois Urbana-Champaign in 2003 and from Rosalind Franklin University of Medicine and Science with a Master of Science degree in Physician Assistant Studies in 2006. She has practiced medicine in a number of different fields as a Physician Assistant since 2006 and has specialized in dermatology since 2015. Brittany’s goal is to provide the highest quality care while still maintaining a compassionate and caring demeanor. She strives to help patients understand their medical conditions and improve their well-being through partnership and education. She states, “It is important that my patients are not only healthy on the inside but confident about their outside as well.“ Her interests include: General Dermatology, Pediatric Dermatology, Acne, Eczema and performing surgical and cosmetic procedures. She also speaks fluent conversational and medical Spanish.
Please call 847-298-1831 to book your BOTOX treatment with Brittany Scurto, PA-C.
All Cosmeceutical Products 25% Off
ONE DAY ONLY

Please call 773-281-9200 for more information or visit our Skin Store.
 Summer sun, sweat and sunscreen can play a toll on our skin. During the month of September, Lakeview Dermatology is offering Glycolic and Salicylic acid peel packages for 3 for $200. Our providers will determine which peel is right for your skin needs. (Consultation is required, offer valid at all Lakeview Dermatology locations)
Summer sun, sweat and sunscreen can play a toll on our skin. During the month of September, Lakeview Dermatology is offering Glycolic and Salicylic acid peel packages for 3 for $200. Our providers will determine which peel is right for your skin needs. (Consultation is required, offer valid at all Lakeview Dermatology locations) September is healthy aging month! All Avene is 15% off throughout the month of September. Avene is infused with spring water, whose beneficial properties have been soothing and effective at relieving skin conditions for more than two and a half centuries. Ask your healthcare provider which Avene products are right for you. Offer valid at all Lakeview Dermatology locations.
September is healthy aging month! All Avene is 15% off throughout the month of September. Avene is infused with spring water, whose beneficial properties have been soothing and effective at relieving skin conditions for more than two and a half centuries. Ask your healthcare provider which Avene products are right for you. Offer valid at all Lakeview Dermatology locations.















Recent Comments